Survival after transplantation – poor average for the lungs
Scientists at the DZL sites Munich and Hanover are searching for causes and therapies for rejection reactions after lung transplantation. In this case however, the immune system of the lung is a curse and a blessing in one.
Chronic end stage lung diseases, such as COPD, cystic fibrosis or pulmonary fibrosis display huge challenges for physicians, because regenerative therapies do not exist. Only lung transplantation can ensure the survival of patients. Unfortunately, new problems often arise after a successful transplantation. The immune system of many patients reacts with rejection to the new lung. In the worst case, frequent, initially acute rejection episodes can further lead to chronic lung allograft dysfunction (CLAD).
The particularly tricky part - once again the vital and complex functions of the lung precisely promote this harmful development:
- As the lungs are responsible for gas exchange, they are constantly connected to the environment, allowing harmful substances to enter the lung.
- In order to ward off harmful substances from the environment, the lung is immunologically extremely active - which unfortunately also intensifies undesirable immune reactions.
- The large surface area of the pulmonary alveoli makes the fight against these undesired immune reactions even more difficult.
As a result, lung transplant patients have the worst long-term survival rate on average.
ECMO lung machine and cytomegalovirus infections
What are the mechanisms behind this rejection and what can be done to prevent or at least mitigate the reaction? Two doctoral students at the University of Munich Hospital (LMU) in the group of DZL-Principal Investigator PD Dr. Gerhard Preissler and Prof. Dr. Rudolf Hatz are doing research on this topic. The project is a cooperation with the DZL-site Hannover (BREATH) under the direction of Prof. Axel Haverich.
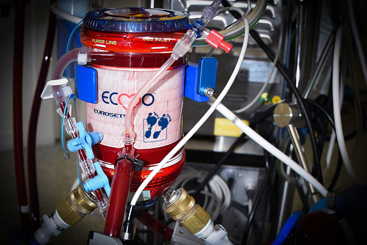
The Biologist Nicole Strobl investigates extracorporeal membrane oxygenation (ECMO). ECMO is a mini lung machine that functions outside the body and takes over the vital gas exchange instead of the lung. It is used in cases of severe lung damage, e.g. COVID-19, but also shortly before or during lung transplantation ("bridge to transplant").
In an observational study, Strobl investigated the consequences of preoperative ECMO-use for the patient. She found out, that patients with ECMO-treatment before transplantation suffered significantly less rejection and thus survival was improved. It is possible that the ECMO device has a kind of recovery effect on the lungs. The immune system is not stimulated as actively and therefore does not turn against itself. This in turn improves the postoperative effects. In the patient groups without ECMO or with ECMO "only" during the operation the result was worse.
These observations lead to the hypothesis: Especially in patients with a critical/difficult preoperative course, the use of ECMO should be considered before surgery.
For this work Nicole Strobl was awarded the Research Prize at the Congress of Thoracic Surgeons in Germany, Austria and Switzerland in 2019.
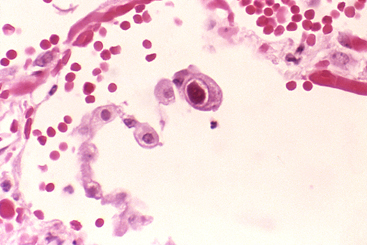
Her colleague Laura Riederer, whose work was also nominated for this research award, pursues another factor that reduces the chance of survival of lung transplant patients: the cytomegalovirus (CMV).
About 60% of the general population are asymptomatic carriers. However, infection with the virus is particularly harmful for patients with a weakened immune system; for example, when the immunological reaction of patients is suppressed after transplantation to protect them from rejection. The body's own defence cells then constantly deal with the virus and the immune system remains stimulated. This often leads to acutely life-threatening episodes of disease with clinically serious consequences.
CMV as a promoter of rejection reactions?
Against this background, Laura Riederer is mainly investigating the alterations in different immune cell populations caused by CMV infection in patients and the effects on the postoperative course. She found out that patients with CMV suffer more often from acute and chronic rejection episodes and show a worse survival compared to patients without viral disease. In the long term, significant changes were observed in different cell types of the immune system.
Interestingly, the first infections caused by CMV occurred very early in the examined patients, within 90 days after lung transplantation. In contrast, cellular changes only became visible with a delay of nine months. These findings were also the subject of a highlight presentation at the DZL Annual Meeting in early 2020.
Identifying high-risk patients earlier and improving therapy
The findings from both studies of the doctoral students raise important questions: Which immunological changes are essential in order to better identify high-risk patients and to be able to use drug therapy after lung transplantation in a more targeted way in the future? Answering these questions will be the next steps in lung research in this field.


